Your Nutritional Guide to Managing Premenstrual Dysphoric Disorder (PMDD)
Premenstrual Dysphoric Disorder (PMDD) is a serious extension of premenstrual syndrome (PMS), affecting 5-8% of menstruating individuals. This condition can be disabling, causing significant distress and functional impairment, impacting work, relationships, and overall well-being. Unfortunately, there is a stigma surrounding PMDD, leading to dismissive attitudes and a lack of understanding.
PMDD is a cyclic mood disorder influenced by hormonal changes, manifesting in the premenstrual or luteal phase of the menstrual cycle and alleviating shortly after menstruation begins. Despite most women with PMDD having normal hormone levels, the disorder is characterised as a heightened sensitivity to the regular fluctuations in female reproductive hormones, akin to how some individuals react positively to alcohol while others may become irritable, aggressive or sad.
The onset of PMDD symptoms typically aligns with the luteal phase, marked by a surge and decline in progesterone levels. This hormonal shift triggers heightened activity in the emotional centre of the brain of women with PMDD in contrast to those without the disorder who usually experience a calming effect during this phase of their cycle. The luteal phase spans approximately 12-14 days, meaning individuals with PMDD face managing symptoms for up to two weeks before transitioning to a phase of damage control until the next cycle of symptoms emerges. For the average woman, this adds up to be up to 8 years of menstruating life spent in this state. Many women describe PMDD as an all-encompassing disorder that significantly challenges daily life navigation. PMDD has been recognised as a distinct clinical entity as the Diagnostic and statistical Manual Of Mental Disorders has officially listed it as a Depressive disorder hoping to provide a framework for understanding, diagnosing and treating the condition.
Photo by Polina Zimmerman
There is no blood, hormone or saliva test to diagnose PMDD but instead tracking symptoms daily for at least two menstrual cycles is recommended. The official criteria for diagnosis is at least 5 of the following 11 symptoms, including 1 of the 4 in bold, which occur during the week before the onset of menses (can be termed the ‘PMDD Hazard Zone’) and are minimal or absent after menstruation:
Depressed mood, feelings of hopelessness or self-deprecating thoughts
Marked anxiety, tension, feelings or being ‘on edge’
Rapid exaggerated changes in mood and emotions
Irritability, anger or increased interpersonal conflict
Decreased interest in usual activities (work, school, friendships, and hobbies)
Difficulty concentrating
Lethargy, marked lack of energy
Change in appetite, specific food cravings, overeating or binge-eating
Hyperinsomnia or insomnia
Feeling overwhelmed or out of control
Physical symptoms such as breast tenderness or swelling, headaches, joint or muscle pain, a sensation of bloating or weight gain assessment.
PMDD may be under-diagnosed and under-treated due to its consistent yet intermittent nature. Risk factors include traumatic events, preexisting anxiety disorders, smoking, and certain genetic variations.
Diagnosis involves a thorough assessment of symptoms, timing in relation to the menstrual cycle, and impact on daily functioning. It is essential for healthcare providers (including gynaecologists, psychiatrists and primary care physicians) to collaborate and conduct a comprehensive clinical assessment, ruling out other conditions.
Photo by Sora Shimazaki
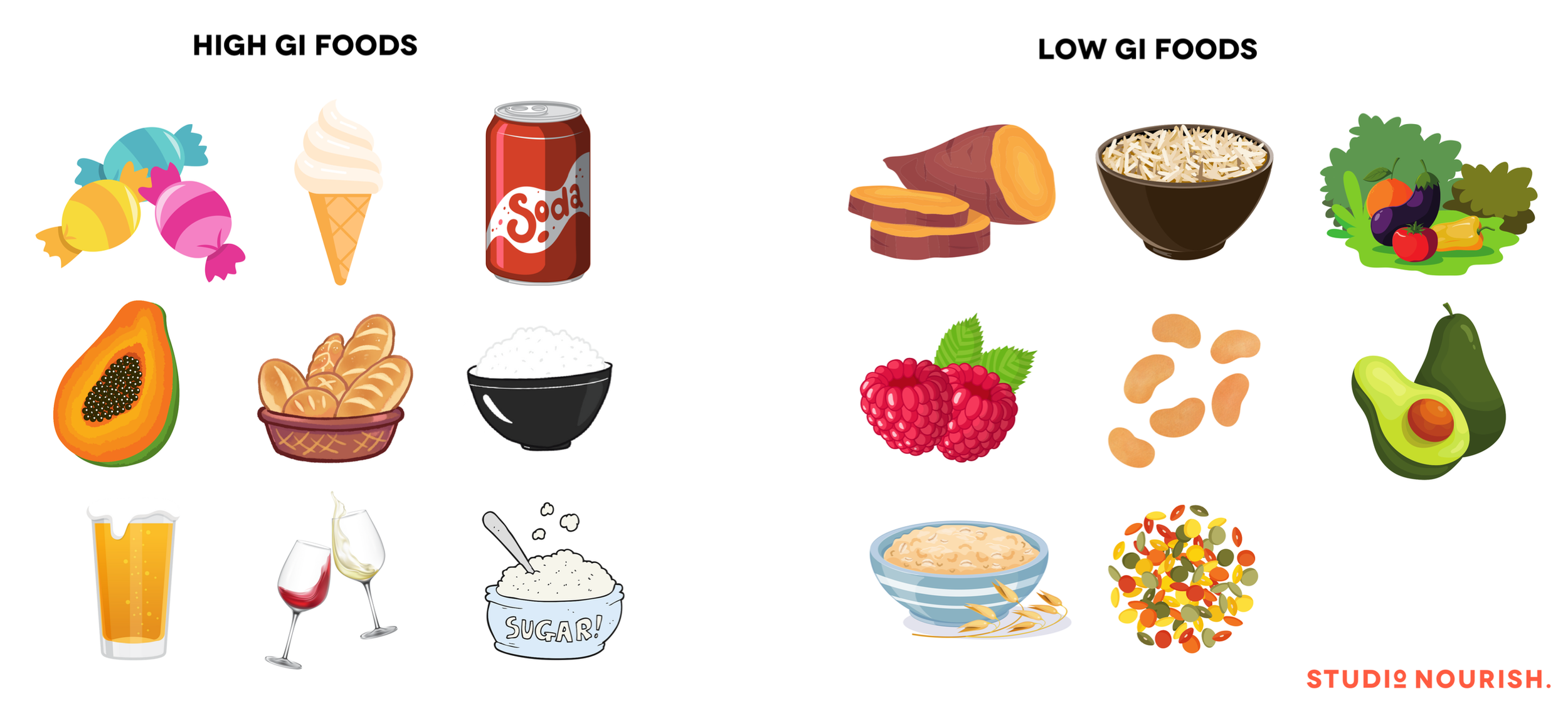
There isn't a one-size-fits-all treatment for PMDD. For moderate cases, non-pharmacological approaches include lifestyle changes, exercise, stress reduction, and a balanced diet. Diets rich in complex carbohydrates (sweet potato, brown rice, quinoa, wholegrain pasta) and proteins, along with calcium-rich foods (dark leafy greens, cauliflower, dairy), may help. Vitamin B6 (tuna, salmon, chickpeas, salmon) could enhance key neurotransmitters such as dopamine which helps to improve emotional well-being and cognitive function.
Exercise has proven more beneficial than another, allowing patients to choose an activity they prefer. Effectively navigating the ‘PMDD Hazard zone’ of the menstrual cycle involves stress reduction or management and improvements in sleep patterns. Stress management strategies may encompass more relaxation time, self-care practices, engaging in hobbies like reading or painting, and incorporating yoga or breathwork into the daily routine.
Because their is such a strong correlation between diet and emotional well-being, it’s crucial to steer clear of refined carbohydrates with simple sugars which have a higher glycemic index (GI)- these include foods such as white bread, white rice, sugar, sweets, pasta and can worsen symptoms.
For individuals experiencing more severe symptoms which remain unalleviated through holistic lifestyle changes, clinical professionals may opt for pharmacological interventions. Medications such as serotonin re-uptake inhibitors (SRIs) or benzodiazepines (BZDs) to ease depressive or anxiety-induced episodes.
Hormonal therapies such as the oral contraceptive and implant are another avenue, aiming to suppress the ovulation stage of the menstrual cycle and prevent the fluctuations in progesterone that trigger symptom onset. Its important to note that while this approach can be effective, it may introduce a set of new symptoms associated with induced medical menopause as menstrual period will stop. It is also masking the symptoms and not addressing the root cause.
Navigating life with PMDD is challenging and requires a comprehensive and individualised approach. A holistic understanding of the disorder is vital for tailored and effective care. Eliminating stigma and fostering awareness about the condition are crucial steps toward providing support. Ongoing research also plays a pivotal role in advancing our knowledge of PMDD.
Photo by madison lavern on Unsplash
If you are experiencing PMDD symptoms and would like support, please reach out to us and book a discovery call to see how nutrition and lifestyle guidance can help you to navigate this condition.
There are also great online resources which can be found at Evelyn Health.